Patient Avoids Open Heart Surgery With Minimally Invasive Bypass
October 21, 2021
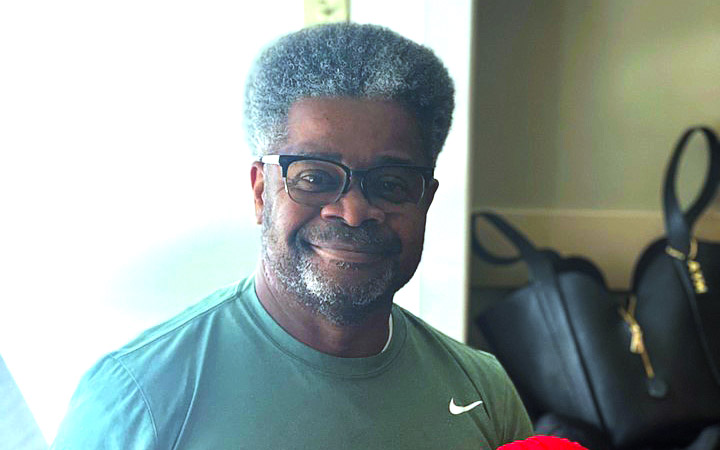
Steve Momon of South Euclid, Ohio is an avid walker. He does five miles per day about four days per week. When he’s not walking through his neighborhood and surrounding areas, he’s walking 18 at the golf course.
“I’m always on the go. I’m always moving,” he says.
But he came to a halt one Monday morning as he set out for his usual route. He suddenly felt tightness in his chest and became fatigued. He made it home and sat down until those unusual feelings subsided. The next day, the same thing happened again.
That Wednesday, he visited his primary care physician, who performed an electrocardiogram and didn’t like the results. Steve went straight to the emergency department of UH Ahuja Medical Center, where he was admitted into the care of cardiovascular experts with UH Harrington Heart & Vascular Institute. His care team discovered he had a blockage in his left anterior descending (LAD) artery.
“Many times, a blockage in the LAD artery is best treated with coronary artery bypass which is typically an open-heart surgery,” says Marc Pelletier, MD, Chief, Division of Cardiac Surgery, UH Cleveland Medical Center, and Director, Heart Surgery Center, UH Harrington Heart & Vascular Institute. “It is a dependable and life-saving procedure. But because we usually need to open the patient’s chest, they can experience some pain, and the recovery is longer because the bone needs to heal.”
Steve qualified to be treated in a different way, with a procedure called a minimally invasive direct coronary artery bypass (MIDCAB).
“A MIDCAB is also used to address a blockage in the LAD artery, but instead of opening the patient’s chest, the surgeon gains access to the heart by making an incision on the left side of the chest and opening a small area between the ribs,” says Pablo Ruda Vega, MD, cardiac surgeon and Medical Director of cardiac surgery at UH Lake West Medical Center. “It’s less invasive and usually causes less pain and holds a shorter recovery.”
Drs. Pelletier and Ruda Vega performed Steve’s procedure at UH Ahuja, eight days after his initial pain during that Monday morning walk.
In the summer 2021, UH began performing these procedures at community hospitals like UH Ahuja, as well as UH Parma Medical Center and UH Elyria Medical Center.
“Traditionally, MIDCABs are only offered at anchor hospitals where patients receive tertiary and quaternary care,” says Mehdi Shishehbor, DO, MPH, PhD, President, UH Harrington Heart & Vascular Institute; Angela and James Hambrick Master Clinician in Innovation; and Professor at the Case Western Reserve School of Medicine.
“We want patients to walk into any University Hospitals facility and receive the same level of care in Elyria, in Parma, on the eastside, that they would at UH Cleveland Medical Center downtown. It’s our mission to bring the highest quality care and procedures closer to where our patients live.”
To maximize efficiency and system resources, some of the high-tech and high-cost instruments for these procedures are housed at UH Cleveland Medical Center and moved to community hospitals as needed. This has led to substantial cost savings while maximizing the potential for innovative surgeries at these community hospitals.
“UH Ahuja was a one-stop shop for me,” Steve says. “I came in through the ER and didn’t have to go anywhere else. It was convenient for my wife. It was much easier for her to drive to and from Ahuja rather than trying to park downtown. I appreciated being closer to home.”
The day after Steve’s procedure, he was up and doing what he loves – walking. But just a few steps at first. Within two to three days of his surgery, he began walking laps around the step-down unit. He was released from the hospital three days after his procedure.
“I’m so grateful I didn’t have to have traditional open-heart surgery,” Steve says. “I had a minimal amount of pain. I’m always thankful for modern medicine. People hear that I had a heart procedure and they think I’m in bed and can’t move, but I’m doing well and truly grateful.”
Related Links
Expanding cardiovascular services across Northeast Ohio is just another example of how UH Harrington Heart & Vascular Institute is enhancing quality and value for patients while investing in community hospitals. Learn more about UH Harrington Heart & Vascular Institute.
Tags: Heart Surgery


